Mission
The mission of our Pediatric Pulmonary Fellowship Program is to train pediatricians from diverse backgrounds to be outstanding pulmonologists who are 1) skilled clinicians with a foundation in physiology, 2) critical thinkers, 3) avid teachers, and 4) physicians who improve care via scholarship and programmatic development.
Program Overview
Established in 1985, our pediatric pulmonary fellowship program has strived to train the next generation of pediatric pulmonologists to develop expertise in clinical care, medical education, and scholarship. As the largest freestanding children’s hospital within a five-state region, we serve children from a large and geographically diverse area, providing our trainees with a breadth of exposure to pediatric pulmonology. The program includes a structured curriculum in addition to an emphasis on individualized training plans (“academic playground”). Our fellows receive high-volume and diverse clinical exposure, robust research training, and mentorship/training from internationally renowned faculty mentors and leaders in the field. There are well established and subsidized programs to support additional research training through the University of Washington School of Public Health if desired.
curriculum in addition to an emphasis on individualized training plans (“academic playground”). Our fellows receive high-volume and diverse clinical exposure, robust research training, and mentorship/training from internationally renowned faculty mentors and leaders in the field. There are well established and subsidized programs to support additional research training through the University of Washington School of Public Health if desired.
Some of the Fellows Favorite Things About Living in Seattle
- Live within one hour of three national parks with access to hikes, beaches and water activities
- Home to six professional sports teams: Sounders (MLS), OL Reign (NWSL), Kraken (NHL), Mariners (MLB), Storm (WNBA), and Seahawks (NFL)
- More than 60 breweries in Seattle (generally specialize in IPAs; Burke Gilman Brewery is across the street from the hospital!)
- Year-round farmer’s market, including world-famous Pike Place and Ballard
- World-class music venues (e.g., Showbox Soto, Tacoma Dome)
- Family-friend zoo, children’s museums, Museum of Flight, Chihuly Museum of Glass, and MOPOP
- Lots of independent coffee shops (we have Starbucks too ?)
- Take a ferry to Victoria, BC or a whale-watching tour to see resident Orcas



The majority of training takes place at Seattle Children’s Hospital -- learn more about our hospital and the children we care for.
Clinical highlights
- Wide breadth of sub-specialty clinics and sites
- Aerodigestive
- Airway and Respiratory Therapy
- Asthma and Allergy (planned start AY2025-2026)
- Bronchopulmonary dysplasia
- Congenital diaphragmatic hernia
- Chest wall and spine disorders
- Cystic fibrosis
- Home ventilation program
- Fontan
- Neuromuscular
- Primary ciliary dyskinesia and non-CF bronchiectasis
- Sickle Cell
- Sleep disorders
- Tracheoesophageal clinic/Esophageal atresia
- Learn from our unique WWAMI (Washington, Wyoming, Alaska, Montana, Idaho) catchment area
- Opportunities to train at diverse clinical sites
- Regional: Everett, Bellevue, Federal Way/South Seattle
- Outreach: Tri Cities and Wenatchee, WA; Bethel and Anchorage, AK
Service Time
| Year | Inpatient Time | Outpatient Time | Research time | Other rotations |
|---|---|---|---|---|
| 1 | 4.5 months | ½ day continuity clinic/week 1-2 subspecialty clinics/week | 5-6 months |
|
| 2 | 2 months | ½ day continuity clinic/week 2-3 subspecialty clinics/week | 9-10 months |
|
| 3 | 2 months | ½ day continuity clinic/week 2-3 subspecialty clinics/week | 9-10 months |
|
Each inpatient week is one week long (Saturday thru Friday).
4 weeks of vacation in each year
Night Call
- VERY unique aspect of our program!

- Weekend PM call by service fellow/Attending
- Weekday PM call from 7pm-7am each night by “off-service” faculty and fellows (Mon-Fri)
- Year 1 fellows included in weekday PM starting after 6 months of fellowship
- Averages out to roughly 1 night call/month
- This system provides time off (pager-free!) overnight while working on-service
Educational Conferences & Curricula
Educational conferences are protected for fellows’ learning
- Journal Club - Weekly; topics include common pulmonary disorders as well as discussions around healthcare disparities/EDI, environmental stewardship, and climate change; each fellows leads JC 4 times per year
- Justice, Equity, Diversity, and Inclusion (JEDI) curriculum
- UW office of healthcare equity foundation courses (e.g., social determinants of health, bystander intervention, bias and microaggressions)
- Journal club months focused on EDI, climate change/sustainability, and healthcare disparities
- Implicit bias training yearly prior to fellow recruitment season
- Advocacy opportunities at local, regional, and national levels
- Radiology/Pathology Conference - Meets monthly; led by expert pulmonary radiologists and lung pathologist, discuss complex cases presented by fellows
- Complex Case Conference – Weekly; faculty/fellows bring interesting/complex cases to review and “ask the expert”. Often led by consult team.
- Multidisciplinary conferences
- BPD Multidisciplinary conference
- Complex Airway & Esophageal Conference
- CDH Conference
- Pulmonary Service (Team 4) Discharge Rounds
- Pulmonary venous stenosis conference
- PFT Interpretation Curriculum – Paired with an attending to review PFTs every 6-8 weeks
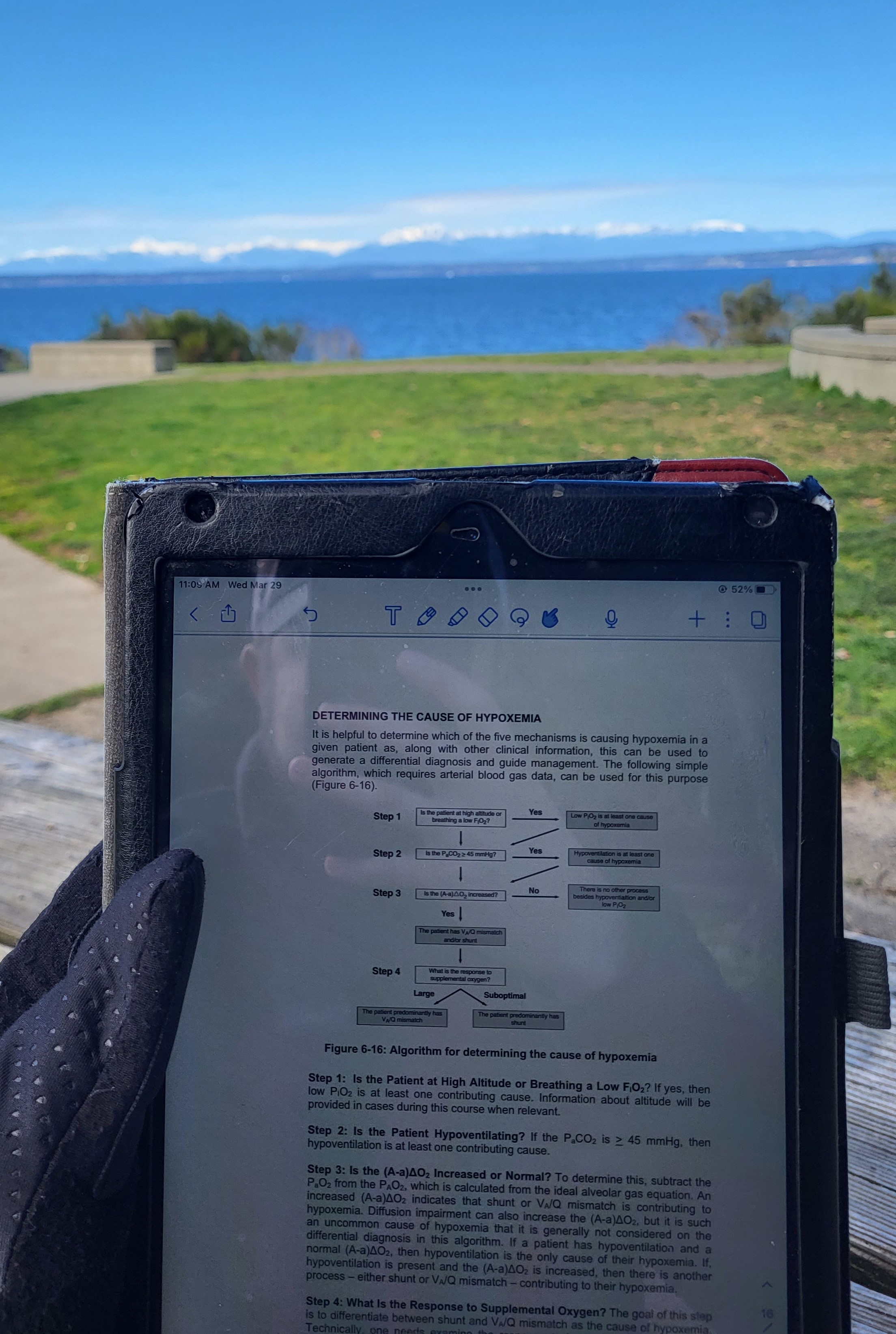
- Pulmonary Physiology Curriculum - Meets 2-3 times/month; interactive syllabus where senior fellows teach core concepts and first-year fellows lead case-based discussions
- Pulmonary Didactics – 2-3 times/month alternating with physiology curriculum; fellow-targeted lectures from faculty within and outside the division
- Western States Conference - Monthly conference that includes other West-coast training programs and led by a pulmonary fellow who presents an unusual case and literature review (each fellow leads one session during fellowship)
- Fellows College - Core educational curriculum and career development services for fellows in all pediatric medical and surgical program at Seattle Children’s Hospital
- Pulmonary Fellows Retreat – Annual retreat each spring for all fellows to support professional development, team building, and wellness
- Opportunities for training and experience in medication education
- Center for Leadership and Innovation in Medical Education (CLIME) seminars and/or Certificate
- Opportunity to be a small group leader for the MS-1 Respiratory and Regulation (R&R) physiology course
- Participate in Pediatric Pulmonary Intern Half-day workshop and monthly “Lunch Bunch” curriculum
- Resident noon conference opportunities
- Wellness/Wellbeing
- Activities (fellowship retreat, fellow appreciation day, super bowl party, etc)
- Wellness resources available (e.g., free counseling you +/- partner, stress management, learning consultation, podcasts, etc.)
Research and Scholarship
- Seattle Children’s Center for Respiratory Biology and Therapeutics (CRBT) launched in 2023
- We promote all fellows to engage in meaningful scholarship during fellowship and help cultivate and develop their own project ideas
- The Arthur Rosenfeld Endowment funds pediatric pulmonary fellowship research
- Conference and travel funds available to attend ~1 conference per year
- Additional intramural travel funds are available for fellows who present their original research
- Opportunities for formal coursework at UW School of Public Health in epidemiology, biostatistics, study design (tuition-exempt)
- Formal coursework on research methods also available at Seattle Children’s Hospital and the Fred Hutchinson Cancer Center (CRISP Summer Program)
- Program Director and Associate Program Director help fellows create their own, individualized mentorship and career development plans
- Opportunities to present at annual Seattle Children’s Hospital fellow and resident research day
Examples of Past/Present Fellow Research Projects
- Rebecca Spurr, MD (Impact of a clinical standard work pathway on management and outcomes of pediatric empyema)
- Drake Bouzek, MD (Using shotgun metagenomics to evaluate the clinical utility of oropharyngeal swabs in children with CF on CFTR modulators)
- Chelsea Davis, MD (Steroid Use in the Treatment of CF Pulmonary Exacerbations) (2021)
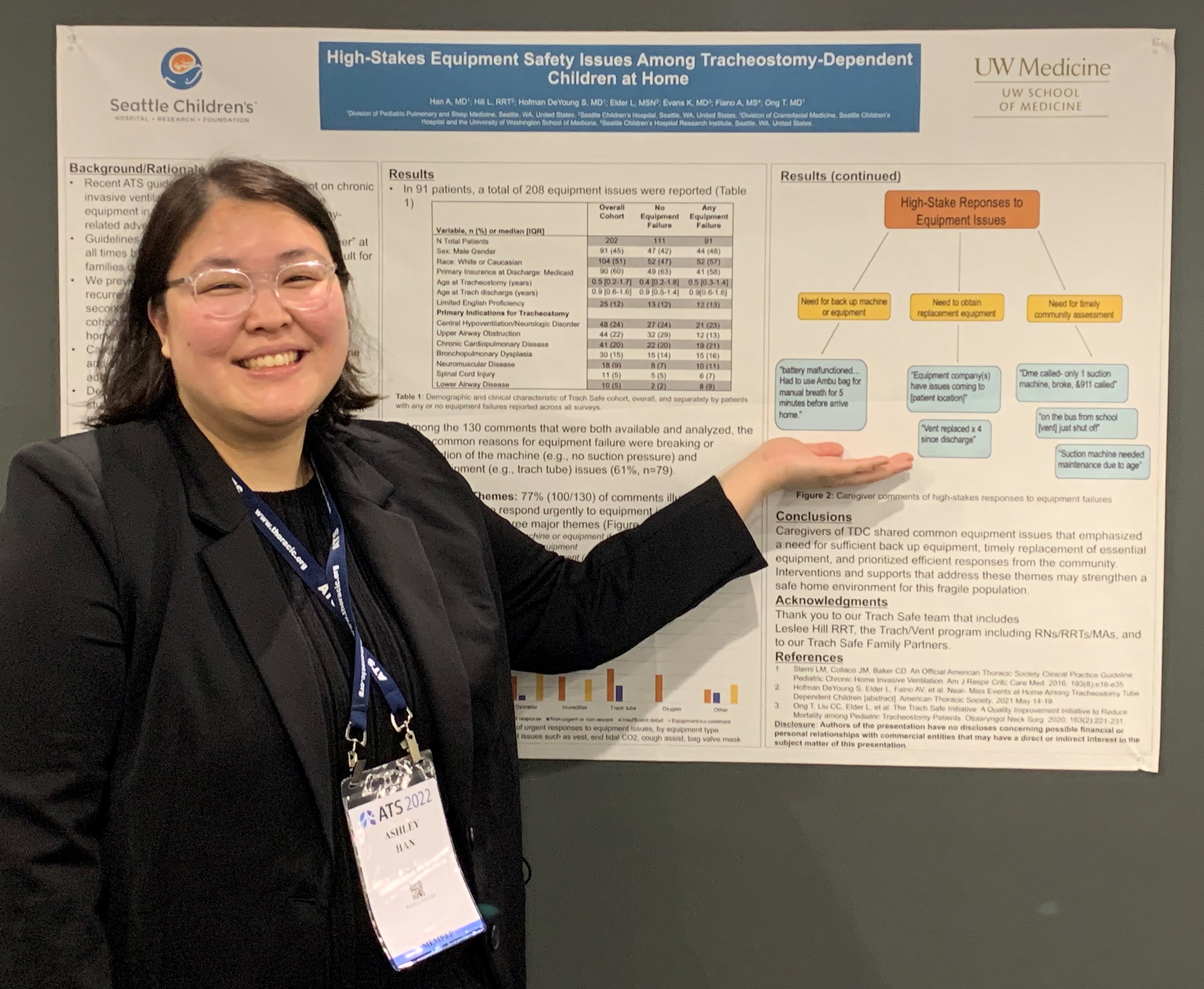
- Sarah Hofman DeYoung, MD (Home Airway Safety Events in Tracheostomy-Dependent Children) (2021)
- Leah Nuss, MD (Transition to Home Ventilators in Patients with Central Airway Malacia) (2022)
- Holly Vo, MD MPH (Decision-Making for Pediatric Home Ventilation) (2022)
- Weston Powell, MD PhD: Airway Epithelial Circadian Rhythms in Pediatric Asthma and Viral Infections (2023)
- Georgene Hergenroeder, MD: Impact of Trikafta on Serum Markers of Fat-Soluble Vitamin Levels in CF (2023)
- Courtney Gallagher, MD: Long Term Outcomes for Children with Congenital Diaphragmatic Hernia with and without Pulmonary Hypertension (2024)
- Ashley Han, MD: Association between childhood opportunity index and healthcare utilization among children with cystic fibrosis (2024)
Requirements
- Prerequisites/post-medical school requirements: U.S. citizen or U.S. permanent resident; board-eligibility in pediatrics
- Must be a graduate of an ACGME-accredited residency program, an AOA-approved residency program, a program with ACGME international (ACGME-I) Advanced Specialty Accreditation, or a Royal College of Physicians and Surgeons of Canada (RCPSC)-accredited or College of Family Physicians of Canada (CFPC)-accredited residency program located in Canada
- Satisfactory completion of a pediatrics or combined internal medicine-pediatrics residency
- Two or more Letters of Recommendation included with your application
- Visa Sponsorship: J1 visa (must be valid through fellowship graduation); H1B Visa in select circumstances
- National Residency Match Program (NRMP).
- All applications must be submitted through the Electronic Residency Application Service (ERAS)
- Register for ERAS
- For questions regarding ERAS, please contact myeras@aamc.org or (202) 862-6264.
Timeline
- Application deadline: August 15, 2025
- Interview Time Period: August 2025 through late October 2025
- NRMP Match Day: November 2025
- Fellowship start date: July 7, 2026
Interview Process
The University of Washington has mandated that all interviews will be conducted online/virtually for the 2025-2026 interview season. We are planning an opportunity for an in-person second look towards the end of the interview season.
Additional Information
Overview
We in the Pediatric Pulmonary Division strive to both create an inclusive environment for ALL people who work at Seattle Children’s Hospital and the University of Washington and provide equitable care for ALL children in our region.
EDI training is ongoing at Seattle Children’s Hospital and the University of Washington. In our division, we have enhanced our EDI training curriculum via seminars, lectures, and dedicated journal club topics in addition to collaboration with the graduate medical education team at the University of Washington.
There are multiple scholarship opportunities available to work with EDI- and healthcare disparities experts and researchers.
Respect for all community members is paramount; bias reporting tools and trainee support are available through Seattle Children’s Hospital and the University of Washington.
Read more about how UW GME is addressing EDI.
Curriculum
- Journal club months focused on healthcare disparities, EDI, and climate change/sustainability
- Implicit bias training yearly prior to fellow recruitment season
- UW office of healthcare equity foundation courses (e.g., social determinants of health, bystander intervention, bias and microaggressions)
- Advocacy opportunities at local, regional, and national levels
- Research opportunities available with experts from Seattle Children’s Hospital and the University of Washington
Division of Pulmonary and Sleep Medicine EDI Committee
- Monthly committee meetings (Division Head Dr. Terri Laguna is Chair of this committee)
- Physical EDI board displaying EDI-related content (updated monthly)
- Faculty recently participated in a novel Bias Reduction in Medicine (BRIM) curriculum
- Divisional collaboration with underrepresented high school students through the Rainier Scholars program
University of Washington and Seattle Children's Hospital
- Health equity rounds (monthly) with a focus on how equity, bias, and racism play out in medical settings
- Culture navigators available for families when needed
- Child Health Equity Research Fellowship available
- Network of underrepresented residents and fellows (NURF)
- UW Department of Pediatrics JEDI committee
Seattle Children's Hospital

Seattle Children's Hospital is both a community hospital for greater Seattle and the pediatric referral center for the Northwest providing excellent pediatric care to meet the medical, surgical and developmental needs of children in the WWAMI region (Washington, Wyoming, Alaska, Montana, and Idaho). Serving as the main clinical training site for pediatric residents, this 423-bed hospital is conveniently located 1.5 miles from the University of Washington campus in a residential neighborhood of Seattle. The staff consists of University faculty and Seattle Children's full-time physicians.
Additional Information
Fellowship Leadership
Terri A. Laguna, MD, MSCS, ATSF
Division Head, Pulmonary and Sleep Medicine Professor Principal Investigator, Center for Respiratory Biology and Therapeutics
Jonathan Cogen, MD, MPH
Associate Professor Director, Pulmonary Fellowship Program Principal Investigator, Center for Respiratory Biology and Therapeutics
Laura Ellington, MD, MS
Assistant Professor Principal Investigator, Center for Respiratory Biology and Therapeutics Associate Director of Pediatric Pulmonary Fellowship



Current Fellows
 | Daphne Cheng, MD (2025-2028) Residency: Seattle Children’s Hospital/University of Washington Cystic fibrosis, asthma, bronchopulmonary dysplasia, technology dependence, health disparities and barriers in access to care in pulmonology |
 | Maddie Peha, MD (2025-2028) Residency: McGaw Medical Center of Northwestern University/Lurie Children’s Hospital
|
Image

| Jessica Clarion, MD (2024-2027) Residency: Tripler Army Medical Center Cystic fibrosis, primary ciliary dyskinesia, non-CF bronchiectasis, airway microbiome, asthma, non-tuberculous mycobacteria, disparities/gaps in newborn screening, pulmonary disease in the military dependent population |
Image

| Jose Carlo Sosa, MD (2024-2027) Residency: Los Angeles Medical Center/USC Aerodigestive disorders, pulmonary complications following bone marrow transplant, technology dependence |
 | Blair Mockler, MD (2023-2026) Residency: Seattle Children’s Hospital/University of Washington Aerodigestive, interventional bronchoscopy, technology dependent children, climate change, non-CF bronchiectasis |
 | MacKenzie Wyatt, MD (2023-2026) Residency: Vanderbilt University |
Alumni
 | Drake Bouzek, MD (2022-2025) Position after Graduation: |
 | Rebecca Spurr, MD (2022-2025) Position after Graduation: |
| Courtney Gallagher, MD (2021-2024) Position after Graduation: Assistant Professor, UW/Seattle Children's Hospital |
| Ashley Han, MD (2021-2024) Position after Graduation: Assistant Professor, Loma Linda Children’s Hospital |
 | Georgene Hergenroeder, MD (2020-2023) Position after Graduation: Assistant Professor of Clinical Pediatrics, Children’s Hospital of Philadelphia |
 | Weston Powell, MD, PhD (2020-2023) Position after Graduation: Acting Assistant Professor, UW/Seattle Children’s Hospital |
 | Leah Nuss, MD (2019-2022) Position After Graduation: Assistant Professor, Tulane University School of Medicine |
 | Holly Vo, MD (2019-2022) Position After Graduation: Acting Assistant Professor, UW/Seattle Children’s Hospital |
 | Sarah Hofman DeYoung, MD (2018-2021) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Chelsea Davis, MD (2018-2021) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | David Panek, MD (2017-2020) Position After Graduation: Assistant Professor, UC-San Francisco |
 | Laura Ellington, MD (2017-2020) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Erin MacKintosh, MD (2016-2019) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | BreAnna Kinghorn, MD, MS (2015-2018) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Jonathan Cogen, MD, MPH (2014-2017) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Laurie Eldredge, MD PhD (2012-2015) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Stephen Reeves MD PhD (2011-2014) Position After Graduation: Assistant Professor, UW/Seattle Children’s Hospital |
 | Kensho Iwanaga MD MS (2010-2013) Position After Graduation: Assistant Professor, UC-San Francisco |
Please follow us on Twitter @UWPedsPulm
Terri A. Laguna, MD, MSCS, ATSF
Division Head, Pulmonary and Sleep Medicine Professor Principal Investigator, Center for Respiratory Biology and Therapeutics
Jonathan Cogen, MD, MPH
Associate Professor Director, Pulmonary Fellowship Program Principal Investigator, Center for Respiratory Biology and Therapeutics
Laura Ellington, MD, MS
Assistant Professor Principal Investigator, Center for Respiratory Biology and Therapeutics Associate Director of Pediatric Pulmonary Fellowship






























