Program Goals
Our Vision: To develop the future leaders in pediatric infectious diseases research, clinical care, and education.
Our Mission: Our fellowship training program prepares individuals to excel as academic physicians, researchers, and leaders in the field of Pediatric Infectious Diseases by providing exceptional research opportunities, diverse clinical and educational experiences, and individualized mentorship.
Research Training
Fellows choose to link with University of Washington faculty members at Seattle Children’s Hospital, Seattle Children’s Research Institute, the University of Washington, or the Fred Hutchinson Cancer Center. The fellowship program assists each trainee to develop their chosen scholarly focus suited to his/her interests that lead to the development of an independent research program.
Clinical Training
Fellows acquire clinical expertise in Infectious Diseases through direct patient care as a consultant, didactic teaching, and participation in conferences. Fellows emerge with extensive experience in management of a wide variety of infections, including bacterial, viral, fungal, and parasitic infections in previously healthy children, as well as surgical and immunocompromised patients.
Prospective Residents & Fellows
- Clinical Training
Clinical Training Settings
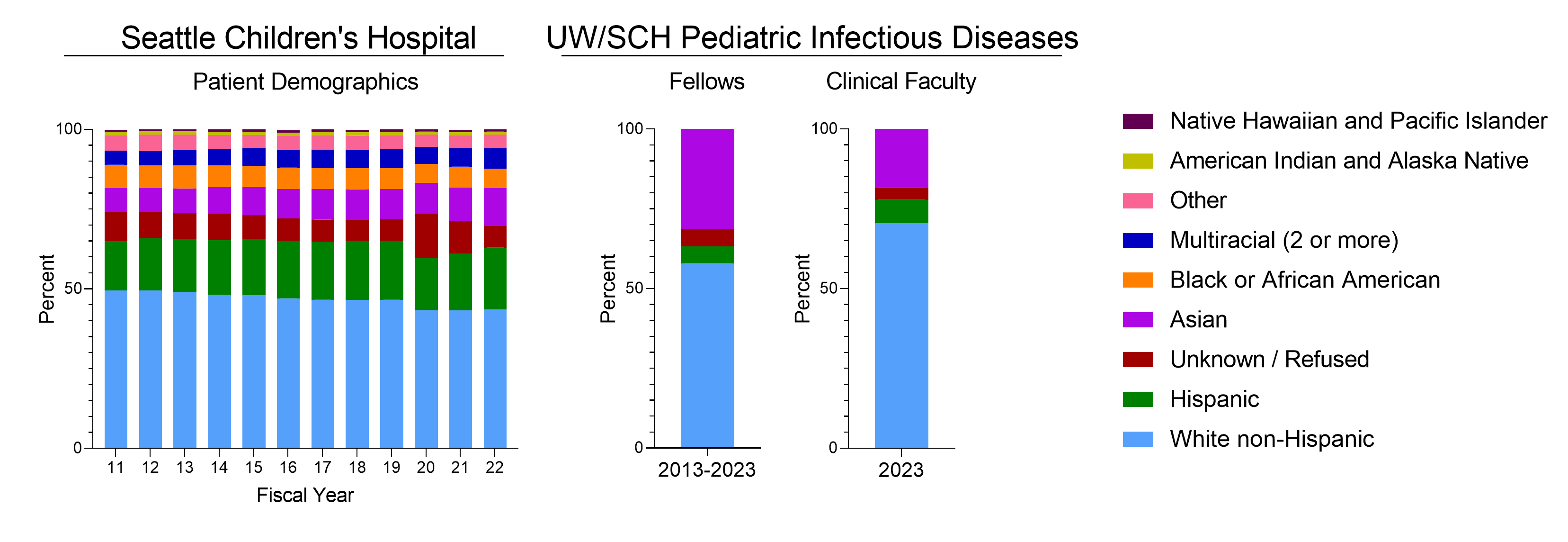
Inpatient Care: The core of the training program is the inpatient service at Seattle Children's Hospital, a quaternary care center with a referral base including five states. Find more data on our patient demographics here. The spectrum of disease is broad, ranging from infections in healthy children to those in bone marrow or solid organ transplantation recipients.
Outpatient Care: Fellows participate in the outpatient management of patients in the General Infectious Diseases, HIV/Virology and Immunology Clinics. Fellows evaluate new consults and provide continuity of care for patients discharged from the inpatient services.
Clinical Laboratory Training: Fellows participate in formal laboratory training sessions in the microbiology and virology labs during their first year. This intensive training experience is complemented by regular interaction with the microbiology labs during the inpatient rotations at Seattle Children's Hospital.
Clinical Training Elements
The majority of clinical training for fellows occurs in the first year of fellowship, but some clinical training can occur during all three training years. This training includes:
Inpatient Consultative Service:
Approximately 40 weeks are spent in Seattle Children’s Hospital inpatient consult service. Additional training may be spent at University-affiliated hospitals including Harborview Medical Center (where the regional trauma and burn units are located) and University of Washington/Fred Hutchinson Cancer Center (FHCRC) Bone Marrow Unit, along with elective rotations arranged on an individual basis.
Clinical laboratory training:
- 2 weeks of rotations in the micro laboratory with experience in diagnostic bacteriology, mycology, and virology laboratories.
Outpatient Clinics:
- Outpatient clinic experiences include general ID clinic, virology clinic, and elective time in immunology clinic.
- Didactic Curriculum
Our Pediatric Infectious Diseases fellowship offers a comprehensive curriculum integrating clinical case discussions with weekly didactic sessions aligned with the American Board of Pediatrics' Pediatric Infectious Diseases content specifications. Alongside approximately quarterly sessions in professional development, grant writing, and Equity, Diversity, & Inclusion initiatives, our program includes weekly clinical cases, city-wide infectious diseases clinical case conferences, and board review topics. Additional monthly activities include journal club and integrated quality improvement/antimicrobial stewardship conferences. Primarily led by faculty and invited experts, fellows also contribute by developing and presenting their own lectures and research conferences, enhancing their teaching portfolio.
- Research Training
A scholarly project is required by the ABP for all fellows completing Pediatric ID fellowship, but the type of work undertaken will vary across fellows and between our Clinician Educator and Academic Research track fellows. Thus, we tailor an individualized program to provide each fellow a strong foundation to build an academic career and result in a scholarly work product as defined by the ABP. Most often fellows achieve this through a publication in a peer-reviewed journal by the completion of fellowship.
Research Training Elements
Mentor Selection: Selection of a research project prior to acceptance to the fellowship program is not required. During the interview process, applicants are exposed to the breadth of faculty expertise available in our program and potential research projects. Upon acceptance into our program, fellows work with the program director and the research director to develop their ideas and research focus further, and begin to identify specific mentors at the University of Washington, Seattle Children’s Hospital, Seattle Children’s Research Institute, or the Fred Hutchinson Cancer Center. Doing so provides fellows extra time to begin learning a new field and considering projects, which helps them use their fellowship time most efficiently. The fellowship director and research director discuss training expectations with both the mentor and fellow to optimize the research project selected by the fellow.
Project Scope: Fellows may work with any University of Washington faculty member including our core pediatric infectious disease faculty listed below. Fellows may select projects related to but not limited to basic science research, epidemiology and population-based research, patient-outcomes research, quality improvement, antimicrobial stewardship, medical education, or global health. Academic Research track fellows are supported by an NIH training-grant to train fellows in basic and/or translational research. Clinician Educator track fellows are supported by Seattle Children’s Hospital. For all fellows, the research project work should be able to be completed within two years and result in a publication in a peer-reviewed journal by the completion of fellowship. For Academic Research track fellows, the project should typically also provide a foundation for a career development grant and future research programs. When needed, our program works closely with fellows to secure funding for a third year of focused research time immediately following fellowship completion.
Coursework: Research is supplemented by coursework at the University of Washington as necessary. Fellows may pursue a master’s degree (such as MPH, MS, etc) if the coursework is appropriate for their career goals. Degree completion takes approximately two years.
Sample Research Trajectory
For Academic Research track applicants, please view attached sample of research trajectory.”
- Research Opportunities
Faculty Mentors
Fellows may choose anyone within Seattle Children’s Hospital or the University of Washington as faculty mentors. This list may not be comprehensive, but does include a wide range of specialties within Seattle Children’s Hospital and the University of Washington.
List of Faculty Mentors (.xls)Additional Resources
- Allergy & Infectious Diseases (AID)
- Seattle Children's Research Division (SCRI)
- Center for Global Infectious Disease Research (CGIDR)
- Center for Clinical and Translational Research (CCTR)
- Fred Hutchinson Cancer Center
- University of Washington - Department of Global Health
- Institute of Health Metrics and Evaluation
Applicants for a position in the pediatric ID fellowship training program should apply through Electronic Residency Application Service (ERAS). Our interview dates for 2026 positions will be between August and November 2025. Selection of applicants will be completed by December 2025 for a July 7, 2026 fellowship start date.
All interviews will be virtual this year, and we are offering 2 total positions to begin in 2026. These 2 positions will be offered in 2 different tracks in the match:
- Academic Research Track: This track can accept up to 2 fellows each year, and is supported by a T32 institutional training grant from the National Institutes of Health (NIH). Per the NIH rules, applicants must be either a United States citizen or permanent resident to be eligible for this support. The goal of this track is to train fellows in Pediatric Infectious Diseases clinical medicine and research, and support them in establishing academic, research-focused careers. Fellows on this track will complete a scholarly project to meet American Board of Pediatrics criteria for Board-eligibility in Pediatric Infectious Diseases.
- Clinician Educator Track: This track can accept up to 1 fellow each year, and is supported by Seattle Children’s Hospital. This track does not have citizenship eligibility requirements. The goal of this track is to train fellows in Pediatric Infectious Diseases clinical medicine and teaching, and support them in establishing academic careers focused on clinical work and teaching. Fellows on this track will also complete a scholarly project to meet American Board of Pediatrics criteria for Board-eligibility in Pediatric Infectious Diseases. Fellows on this track will be supported in pursuing an additional focus of training if they wish. Additional potential areas include, but are not limited to, infection prevention, antimicrobial stewardship, epidemiology and public health, global health, medical education, and transplant infectious diseases.
Those who come from under-represented backgrounds in academic pediatrics are strongly encouraged to apply to our programs. Seattle Children's Hospital is an equal opportunity employer.
Documents to submit via ERAS include:
- The completed Common Application Form
- At least 3 letters of recommendation (including a program director's letter)
- A personal statement about why you are interested in a career in infectious disease
- A photograph
- USMLE and /or COMPLEX transcripts
- MSPE/Dean’s letter and medical school transcripts
Applications must be submitted online using the Electronic Residency Application Service (ERAS).

Land Acknowledgment
We acknowledge that we live and work on the ancestral land of the first people of Seattle, the Duwamish People past and present. We honor with gratitude the land and the Duwamish Tribe.
Our Values
We believe that the diversity of our fellows, residents, medical students, staff, and faculty is of fundamental importance in our ability to ensure that all our patients and families receive the highest-quality care – no matter their race, ethnicity, language, literacy, age, gender, gender identity, sexual orientation, religion, disability, or finances. Our objective is to create a community that encourages participation and connection, one that seeks out and celebrates the unique contributions of each individual, in every aspect of our practice and mission.

Our Community
The Division of Infectious Diseases includes a diverse community with a wide range of backgrounds and identities. Social and professional activities center around the fellows and their training, but also extend to broader affinities beyond the walls of the hospital and research institute. The Division organizes a coffee break every 1-2 weeks for on-service teams and others working in the hospital. Fellows and young faculty gather approximately once a quarter for a happy hour and informal mentoring. As a division we typically come together monthly for holidays, graduation, retirement parties and other celebrations. Additional social and mentorship opportunities are available through the UW Network of Underrepresented Residents and Fellows, Seattle Children’s Fellows’ College and the UW School of Medicine GME Office.
The larger geographic area of Seattle and King County contains a diverse array of cultural, religious, and affinity-based communities. As pediatric infectious diseases specialists, we both serve and participate in these communities actively.
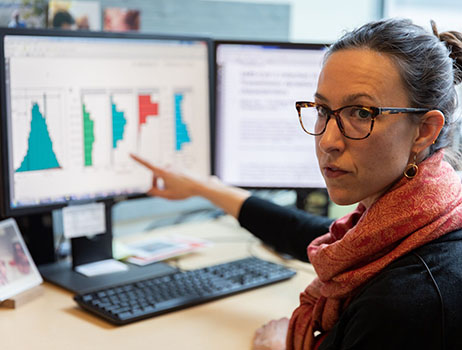
Anti-Racism and Health Equity Work
We recognize that structural manifestations of racism and other forms of prejudice exist in the institutions and society around us; as a division and a fellowship training program we are actively working to dismantle systemic injustice and to increase equity. Some of our ongoing projects are listed below.
- The Infectious Diseases Division incorporates an equity assessment into the development of our clinical care guidelines, quality improvement work and morbidity and mortality conferences. We have adapted a model based on the Equity Impact Tool implemented by King County and others to assess the consequences of our policies and any proposed changes on marginalized groups.
- Through research, advocacy, and action, members of the Division are actively engaged in work to improve health equity both in the United States and globally. Some of these projects are listed below.
- Caitlin McGrath studies the social determinants of health in healthcare-associated infections, investigating racial and language inequities in the incidence of central line-associated bloodstream infections and surgical site infections and strategies for improvement. She was awarded the prestigious Leadership in Epidemiology, Antimicrobial Stewardship, and Public Health (LEAP) fellowship in 2022-2023 to continue this work.
- Jon Mosser studies neglected tropical diseases and vaccine-preventable illness at the Institute for Health Metrics and Evaluation, focusing on the use of computer modeling to maximize the effectiveness of targeted public health interventions in low-resource settings.
- Ben Gern is a mentor in the TB Scholars Program, which provides research experiences and mentorship for undergraduates from underrepresented backgrounds in science who are interested in Tuberculosis research. He is also the recipient of a mentored scholars grant from the SCH Center for Diversity and Health Equity.
- Indi Trehan works with global partners including WHO, UNICEF, MSF, and Action Against Hunger to study and improve the care of malnourished children worldwide. He has extensive experience and interest in training health care providers in austere settings in evidence-based, cost-effective clinical care and public health that maximizes child survival and human potential.
- Taylor Hendrixson is board-certified in both neonatology and pediatric infectious disease. His work focuses on improving maternal-neonatal health and nutrition in resource-poor settings.
- Recognizing the disparity in the racial and economic background between physicians and the patients they serve, the Division participates in several interventions aimed at improving the pathways for individuals from diverse backgrounds to obtain training in medicine. These include the Washington State Opportunity Scholarship, the Summer Scholars Program (SSSP) - Seattle Children's, and Funded Visited Electives . We are actively recruiting at all training levels to improve the diversity of our specialty. If you are interested in exploring any aspect of pediatric infectious diseases, please get in touch with us.
Additional Resources
We are fortunate to have a number of outstanding resources for anti-racism and equity work in our community, including the following.
- UW Medicine Office of Health Equity
- Network of Underrepresented Residents and Fellows
- UW Department of Pediatrics Associate Vice Chair for Equity, Diversity and Inclusion, Dr. Jason Deen.
- UW Department of Pediatrics Justice, Equity, Diversity and Inclusion (JEDI) Committee.
For fellows who are interested in pursuing research in equity-related areas of infectious disease, the University of Washington School of Medicine funds a two-year Child Health Equity Research Program for Post-doctoral Trainees (CHERPP-T) supporting mentored, research project-based training program in health equity research that may be applicable to interested fellows.
We support the University of Washington’s pledge against racism and Diversity Blueprint and the Seattle Children’s Anti-Racism Action Plan to fight and dismantle systemic racism within our institutions, our policies, and our practice of medicine.
Seattle Children's Hospital

Seattle Children's Hospital is both a community hospital for greater Seattle and the pediatric referral center for the Northwest providing excellent pediatric care to meet the medical, surgical and developmental needs of children in the WWAMI region (Washington, Wyoming, Alaska, Montana, and Idaho). Serving as the main clinical training site for pediatric residents, this 423-bed hospital is conveniently located 1.5 miles from the University of Washington campus in a residential neighborhood of Seattle. The staff consists of University faculty and Seattle Children's full-time physicians.
Additional Information
Seattle Children's Research Institute (SCRI)

As one of the nation's top five pediatric research centers, Seattle Children's Research Institute is dedicated to providing hope, care and cures to help every child live the healthiest and most fulfilling life possible. With one million square feet of clinical, laboratory and office space, a workforce of over 2,400 people and over $253 million in total extramural funding for the 2023 fiscal year, we are working toward the next wave of lifesaving discoveries.
The research institute is organized into centers, specializing in areas that include immunotherapy, tissue and immune transplantation, outcomes research, clinical and translational research, and child health and behavior. Researchers work in close collaboration with one another, their colleagues at partner institutions including the University of Washington and Fred Hutch Cancer Center and our healthcare providers at Seattle Children's Hospital. This collaboration allows our faculty to draw on a variety of disciplines and techniques as they pursue solutions to some of medicine's most complex problems.
Harborview Medical Center

Harborview Medical Center (HMC) is one of the nations leading academic medical centers and the only Level I adult and pediatric trauma center serving Washington, Alaska, Montana and Idaho. Harborview Medical Center cares for potential neurosurgical cases of abusive head trauma, all serious burns and trauma and adult and child victims of sexual assault. The medical center is owned by King County and managed by the University of Washington. Harborview has a specific mission to care for the community's most vulnerable patients. Fellows see consults at HMC in the PICU, burn unit, ED and pediatric unit.
Fred Hutch Cancer Center

Fred Hutch Cancer Center is one of the world's premiere research institutions, home to three Nobel Laureates (including Dr. Donnall Thomas, who was awarded the Nobel Prize in 1990 for his contributions to the field of bone marrow transplantation) and many other global leaders in life sciences research. The Center receives more research funding from the National Institutes of Health than any other public or private research institution in the world. The Hutchinson Center, together with its clinical and research partners, the University of Washington and Seattle Children's, comprise the Fred Hutch/University of Washington Cancer Consortium. The Consortium is among 40 National Cancer Institute-designated comprehensive cancer centers nationwide. More than 2,760 people work for the Hutchinson Center, including over 650 scientific faculty and more than 550 pre-doctoral and post-doctoral researchers and other scientific staff.
UW Medical Center - Montlake (UWMC)

UWMC is consistently ranked among the nation's best general hospitals. As the only comprehensive clinical, research and learning health system in the five-state WWAMI (Washington, Wyoming, Alaska, Montana, Idaho) region, UW Medicine provides a higher degree of healthcare, ranging from primary and preventive care to the most highly specialized care for the most complex medical conditions.
From first of their kind, life-saving surgical procedures to routine adult, maternal and newborn medicine, we're training the next generation of medical professionals. By using the latest advances in medical technology and patient- and family-centered care, we're building a better future for our community.
Fellowship Leadership
Yasaman Fatemi, MD, MSHP
Assistant Professor Associate Medical Director, Infection Prevention at Seattle Children’s Hospital Fellowship Program Director, Pediatric Infectious Diseases

Current Fellows
 | Annalise Edan, MDAnnalise is the newest UW/SCH Pediatric Infectious Diseases fellow, joining us in 2025 after completing Pediatric residency at the University of South Carolina. Annalise is interested in public and global health, particularly exploring the intersection of social determinants of health and infectious disease. After receiving their multi-disciplinary BA in 2012, Annalise worked with Keep America Beautiful as an AmeriCorps member before joining the staff of Teach For America – Memphis. Experiences there, including volunteering in the BMT unit at St. Jude, eventually led to a career pivot into medicine; Annalise graduated from the University of Tennessee Health Science Center in 2022. |
 | Hassan Jamal, MBBS, DTM&HHassan is originally from Saudi Arabia, where he completed medical school at King Abdulaziz University. He then completed his pediatric residency and Pediatric Infectious Diseases fellowship at The Hospital for Sick Children/University of Toronto, Canada. He is joining Seattle Children’s Hospital/University of Washington for his third year of fellowship, with a focus on infections in immunocompromised hosts and antimicrobial resistance. Beyond the gravitational pull of Planet Hospital, he finds joy in spending time with family, playing racquet sports, and immersing himself in the wonders of the great outdoors. |
 | Amin Bemanian, MD PhDAmin is originally from the Chicago area and completed his medical and graduate education at the Medical College of Wisconsin in Milwaukee. He completed his pediatric residency training at Seattle Children's Hospital/University of Washington and is excited to stay here for fellowship. His research interests include the intersection of public health and infectious disease epidemiology, and he will be joining Dr. Trevor Bedford’s lab for his fellowship research. Outside of work, Amin enjoys hiking, running, and nature photography.
|
 | Cassie Simonich, MD PhDDr. Simonich completed the University of Washington MSTP and pediatrics residency at Seattle Children’s Hospital. Her research interests include viral evolution and immune evasion. Outside of work, she can usually be found adventuring with her husband, daughter and dog. She might also be found tending to their “backyard farm." |
Alumni




Graduates of our program pursue careers in research and clinical care related to Pediatric Infectious Disease. Approximately 90% of graduates from our program in the past 15 years are conducting research related to infectious disease or are academic pediatric infectious disease physicians. Fifteen of these recent graduates obtained mentored research development awards (K-series from the NIH or their equivalent) in areas related to their fellowship projects.
Publications and Presentations from recent fellowship graduates (2020-2025)
- Sara Ruth Kim, Elizabeth M Krantz, Khaleel Yahya, Terry Stevens-Ayers, Chikara Ogimi, Janet A Englund, Michael Boeckh, Alpana Waghmare, Viral epitope profiling of hematopoietic cell transplant recipients with respiratory syncytial virus upper respiratory tract and lower respiratory tract infections, Journal of the Pediatric Infectious Diseases Society, Volume 13, Issue Supplement_4, October 2024, Pages 30–31, doi: 10.1093/jpids/piae093.079
- Sara Ruth Kim, Anna Nordlander, Hu Xie, Yae-Jean Kim, Chikara Ogimi, Monica S Thakar, Wendy Leisenring, Janet A Englund, Michael Boeckh, Alpana Waghmare, The Impact of Pretransplant Respiratory Virus Detection on Posttransplant Outcomes in Children Undergoing Hematopoietic Cell Transplantation, Clinical Infectious Diseases, Volume 79, Issue 3, 15 September 2024, Pages 761–771, doi: 10.1093/cid/ciae216
Brandon Maust, MD
- Byrne A, Diener C, Brown BP, Maust BS, Feng C, Alinde BL, Gibbons S, Koch M, Pollara J, Gray CM, Jaspan HB, Nyangahu DD. Neonates HIV-exposed and uninfected exhibit an altered gut bacteriome and DNA virome in the first month of life that associates with systemic inflammation. Microbiome. 2024 Dec 20; 12(261)
- Maust BS, Feng C, Brown BP, Happel AU, Jimoh AO, Claassen-Weitz S, Dabee S, Minot SS, Jaspan HB, Varsani A. Genetic Diversity in Viruses of Human-Infecting Protozoa. 2024. International Society for Viruses of Microorganisms Viruses of Microbes 2024. Poster.
- Maust BS, Rametse CL, Feng C, Kamenz D, Byrne A, Mndini M, Alinde B, Ganief Y, Muller E, Maseko V, Lorenzo Redondo R, Amaral Russo T, Gray CM, Hope TJ, Jaspan HB. Changes in penile microbiome of South African cis-gender men and transwomen following surgical circumcision. 2024. 5th HIV Research for Prevention Conference: Lima, Peru. Poster.
- Happel AU, Balle C, Havyarimana E, Brown B, Maust BS, Feng C, Yi BH, Gill K, Bekker LG, Passmore JS, Jaspan HB, Varsani A. Cervicovaginal Human Papillomavirus Genomes, Microbiota Composition and Cytokine Concentrations in South African Adolescents. Viruses. 2023 Mar 15;15(3):758. doi: 10.3390/v15030758. PMID: 36992467; PMCID: PMC10054107.
- Maust BS, Petkov S, Herrera C, Feng C, Brown BP, Lebina L, Opoka D, Ssemata A, Pillay N, Serwanga J, Seatlholo P, Namubiru P, Odoch G, Mugaba S, Seiphetlo T, Gray C, Kaleebu P, Webb E, Martinson N, Chiodi F, Fox J, Jaspan HB. Bacterial Microbiome and Host Inflammatory Gene Expression in Foreskin Tissue. Heliyon. 2023 Nov 14;9(11)
- Happel AU, Balle C, Maust BS, Konstantinus IN, Gill K, Bekker LG, Froissart R, Passmore JA, Karaoz U, Varsani A, Jaspan H. Presence and Persistence of Putative Lytic and Temperate Bacteriophages in Vaginal Metagenomes from South African Adolescents. Viruses. 2021 Nov 23;13(12)
- Maust BS, Feng C, Rametse CL, Mndini M, Alinde B, Ganief Y, Muller E, Maseko V, Lorenzo Redondo R, Amaral Russo T, Gray CM, Hope TJ, Jaspan HB. Urethral microbiome of South African cis-gender men and transwomen with and without bacterial sexually transmitted infections. 2023. IAS Conference on HIV Science: Brisbane, Australia.
- IDWeek, Washington, DC (2022). Poster presentation: “Health Behavioral Trends and Absenteeism Associated with Acute Respiratory Illness Before and During the SARS-CoV-2 Pandemic in a Community Household Study, King County, Washington”
- Chung E, Magedson A, Emanuels A, Luiten K, Pfau B, Truong M, Chow EJ, Hughes JP, Uyeki TM, Englund JA, Nickerson DA, Lockwood CM, Shendure J, Starita LM, Chu HY. SARS-CoV-2 Screening Testing in Schools: A Comparison of School- Vs. Home-Based Collection Methods. J Pediatric Infect Dis Soc. 2022 Dec 5;11(11):522-524. doi: 10.1093/jpids/piac097. PMID: 36082698; PMCID: PMC9494399.
- Chung E, Chow EJ, Wilcox NC, et al. Comparison of Symptoms and RNA Levels in Children and Adults With SARS-CoV-2 Infection in the Community Setting. JAMA Pediatr. Published online June 11, 2021. doi:10.1001/jamapediatrics.2021.2025
- Invited Speaker. “Pediatric ID Fellow Virtual Clinical Case Conference in the Immunocompromised Child.” Pediatric Infectious Diseases Society Transplant Subcommittee.
- McDaniel CE, Jacob-Files E, Deodhar P, McGrath CL, Desai AD. Strategies to Improve the Quality of Team-Based Care for Neonatal Abstinence Syndrome. Hosp Pediatr. 2021;11(9):968-981. doi:10.1542/hpeds.2020-003830
- Bartlett AH, Ravin KA, Rubin LG, McGrath C, de St Maurice A, Linam WM, Logan LK, Muller M, Caughell C, Ramirez-Avila L. SHEA Pediatric Leadership Council Commentary: Inpatient Visitor Considerations for Pediatric Patients during the COVID-19 Pandemic [published online ahead of print, 2021 Jun 11]. Infect Control Hosp Epidemiol. 2021;1-9. doi:10.1017/ice.2021.243
Christine Anterasian, MD
- Crane C, Loop L, Anterasian C, Geng B, Ingulli E. Balancing B cell responses to the allograft: implications for vaccination. Front Immunol. 2022 Jul 27;13:948379. doi: 10.3389/fimmu.2022.948379. PMID: 35967363; PMCID: PMC9363634.
- Anterasian C, Warr AJ, Lacourse SM, Kinuthia J, Richardson BA, Nguyen FK, Matemo D, Maleche-Obimbo E, John Stewart GC, Hawn TR. Non-IFNγ Whole Blood Cytokine Responses to Mycobacterium tuberculosis Antigens in HIV-exposed Infants. Pediatr Infect Dis J. 2021 Oct 1;40(10):922-929. doi: 10.1097/INF.0000000000003254. PMID: 34525006; PMCID: PMC8443847.
Caleb Stokes, MD, PhD
- Hao L, Hsiang TY, Dalmat RR, Ireton R, Morton JF, Stokes C, Netland J, Hale M, Thouvenel C, Wald A, Franko NM, Huden K, Chu HY, Sigal A, Greninger AL, Tilles S, Barrett LK, Van Voorhis WC, Munt J, Scobey T, Baric RS, Rawlings DJ, Pepper M, Drain PK, Gale M Jr. Dynamics of SARS-CoV-2 VOC Neutralization and Novel mAb Reveal Protection against Omicron. Viruses. 2023 Feb 14;15(2):530. doi: 10.3390/v15020530. PMID: 36851745; PMCID: PMC9965505.
- Rodda LB, Netland J, Shehata L, Pruner KB, Morawski PA, Thouvenel CD, Takehara KK, Eggenberger J, Hemann EA, Waterman HR, Fahning ML, Chen Y, Hale M, Rathe J, Stokes C, Wrenn S, Fiala B, Carter L, Hamerman JA, King NP, Gale M Jr, Campbell DJ, Rawlings DJ, Pepper M. Functional SARSCoV-2-Specific Immune Memory Persists after Mild COVID-19. Cell. 2021 Jan 7;184(1):169-183.e17.doi: 10.1016/j.cell.2020.11.029. Epub 2020 Nov 23. PMID: 33296701; PMCID: PMC7682481. Chow EJ, Maust B, Kazmier KM, Stokes C. Sinus Bradycardia in a Pediatric Patient Treated With Remdesivir for Acute Coronavirus Disease 2019: A Case Report and a Review of the Literature. J Pediatric Infect Dis Soc. 2021 Oct 27;10(9):926-929. doi: 10.1093/jpids/piab029. PMID: 34173663; PMCID: PMC8557381.
Yasaman Fatemi, MD, MSHP
Assistant Professor Associate Medical Director, Infection Prevention at Seattle Children’s Hospital Fellowship Program Director, Pediatric Infectious Diseases
Email